Inpatient Unit Design: Defining the Design Characteristics of a Successful Adaptable Unit
RESEARCH TEAM
Debajyoti Pati (PI) and Tom Harvey
COLLABORATORS
Carolyn L. Cason, PhD, Professor, School of Nursing, University of Texas, Arlington, TX
Doug Bazuin, Researcher, Herman Miller, Zeeland, MI
FUNDS
AIA Research Grant 2006 and Herman Miller Grant
AWARDS
Best International Research Project Award, International Academy for Design and Health, Singapore, 2009
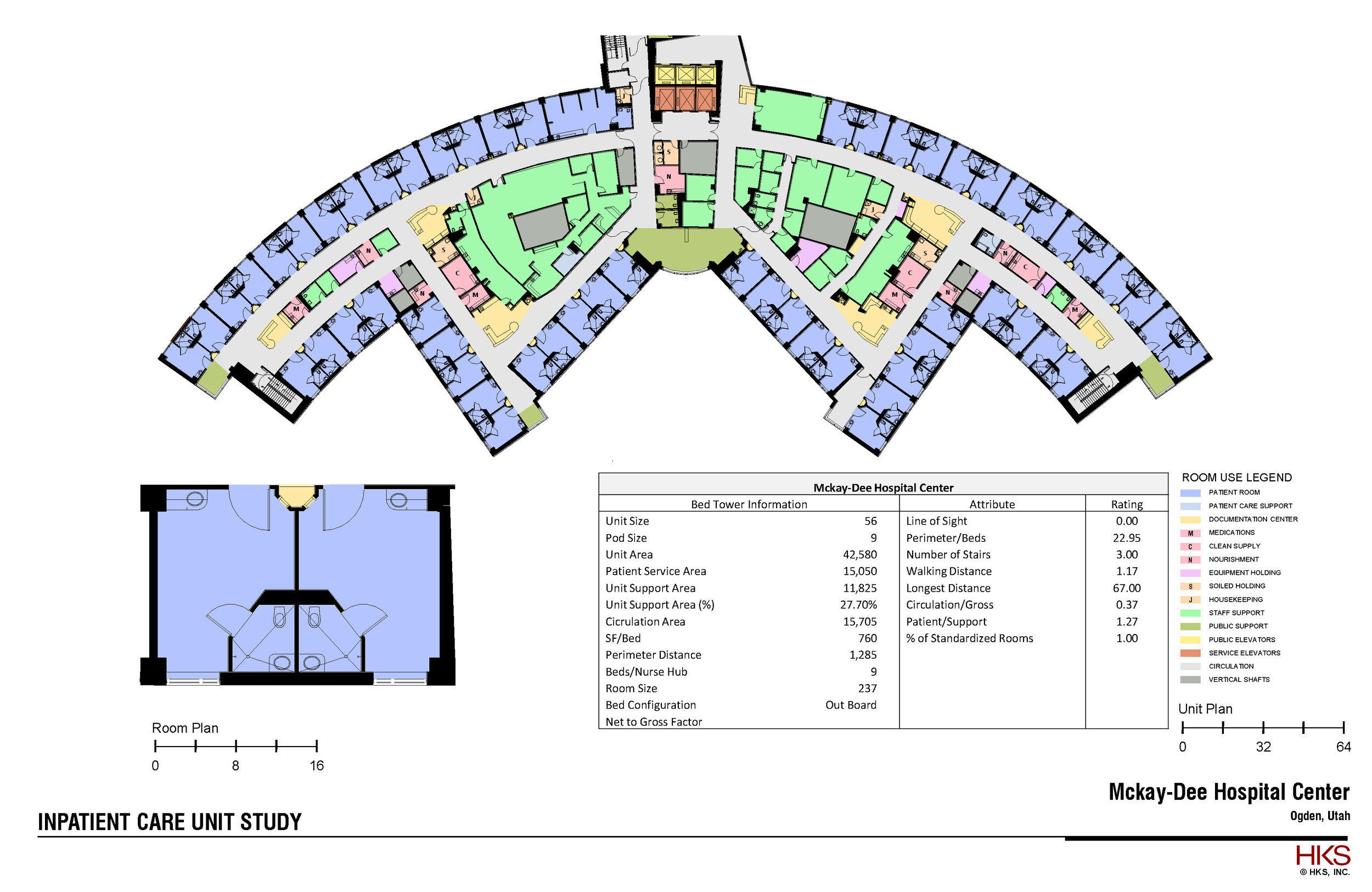
WHAT was the aim
In view of the massive investment being made into inpatient units, this research aimed at ascertaining: 1) what flexibility means to different stakeholders of care delivery, 2) what physical design variables stakeholders identify as dimensions of architecture that influence flexibility, and 3) what elements of the designs promote or hinder flexibility. Existing literature discuss flexibility mostly at the hospital or the patient room level. Moreover, typical flexibility considerations have centered on convertibility and expandability. This study makes a contribution at understanding flexibility at the inpatient unit level, from a viewpoint of adaptability to operational changes.
Why is it important
Healthcare is perhaps going through one of the most challenging phases in U.S. history, with an aging population, rising acuity, growing consumer expectations, a tighter labor market, and advancing technology. Hospitals continuously respond to such changes by implementing changes in unit operational models. The physical design of a unit could facilitate or impede the implementation of such changes, thereby affecting efficiency, stress, and renovation cost.
WHAT DID WE DO | HOW DID WE DO IT
The study used an exploratory design and collected data through semi-structured interviews of stakeholders in nursing, materials management, respiratory services, pharmacy, environmental services, and dietary services from six hospitals across the United States.
What did we find
Content analysis of interview transcript suggests a set of seven ‘static’ attributes the presence of which, irrespective of size, shape, circulation, and other configurations, would ensure flexibility of operations in the short as well as long run: 1) multiple division/zoning options, 2) peer lines of sight, 3) patient visibility, 4) centrality of support, 5) resilience to move/ relocate/interchange units, 6) multiple administrative control and unit spread options, and 7) ease of movement between units and departments. Our findings suggest that the nature of flexibility required could change depending on the specific setting. In addition, adaptability considerations for inpatient care units should be accorded higher, or at least equal, priority to expandability and convertibility. As a result, for designers of inpatient units, adaptability is a vital area to ensure short- and long-term operational efficiency (without de-emphasising the importance of support core convertibility and expandability). Data analyses suggest that physical design plays a crucial role in facilitating or impeding the ability of organisations and their personnel to adapt to changing workload demands, staffing patterns and operational challenges. Adaptability is also crucial to long-term flexibility in inpatient care. Irrespective of changes in technology, operational design, philosophy of service and models of care, several things will remain constant over time in care-giving.
What is next
Future studies could and should begin to link micro and macro flexibility needs and the design issues arising out of such needs. Nevertheless, this paper constitutes a unique and important contribution to our understanding of flexibility in architectural design for inpatient care units.